Early Cancer Detection and Big Data - Health Nucleus Interview Part 1
Shaking hands with Dr. Duchicela (left) during my January 2020 visit to the Health Nucleus!
In this post you’ll learn:
Dr. Duchicela’s background
Big Data & healthcare
The definition of ‘Healthy’
Early detection of Cancer
Part 1 - Intro, Cancer Detection, What is Healthy?
In a series of three posts, Longevity Blog interviews Dr. Keegan Duchicela, Medical Director at the Health Nucleus in San Diego, California. Dr. Duchicela received his medical degree from UCSF in 2007. Since the completion of his residency, he has served as the Lead Physician at the Google Wellness Center (Google’s on-campus medical facility), and over the past three years has held several roles at the Health Nucleus including Clinical Director, Medical Director and Physician.
This interview, from the 24 January 2020, walked through a series of pre-written questions with Dr. Duchicela, and is presented in the form of a transcribed audio conversation.
Longevity Blog:
Q: What motivated you to become the medical director at the Health Nucleus? That’s a pretty cool job!
Dr Duchicela:
A: It is pretty cool! My training is in family medicine, so from the get go I have felt there is great value in preventing and detecting disease before it happens and having actual relationships with the patients to really delve into things other than just normal lab values and imaging. I think you really need to get to know the patient, their family, their socioeconomic context, and their culture, as well as where they live to really get a general sense of their health risks, because there are so many other things besides just labs that determine how healthy you are.
Corporate wellness centers, like those run by Premise Health, are becoming more common at big tech companies, like Google. And they recruit top-notch medical practitioners like Dr. Keegan to run them. Source
I come from a different perspective, I didn’t go into medicine to learn about genetics or advanced imaging or even precision medicine, my focus was more on getting to know the person holistically to really enable them to take care of their body, their mind and their family. I looked at health in that context. But as I went through training and through the kinds of places I’ve worked over my career; I worked for a few years at Google helping lead their onsite primary care clinics where I encountered a lot of interesting individuals, engineers who were doing some amazing things with Big Data, I started to really see the value in having a large data set on health metrics and what you can do with that sort of information and the impact you can achieve. I began thinking that the future of medicine for physicians is as good data scientists with excellent bedside manner.
If we could offer this testing at a very inexpensive price point to millions of people, how much better would our health improve overall? I think it could be pretty dramatic to be honest with you.
I really think that’s where we’re heading. And so as a physician I feel like it’s really important to grasp the implications of using Big Data and what it really means and how we can use these analytical tools to predict where we’re going with our health.
after I left Google, I was looking for a company that was doing innovative things
So after I left Google, I was looking for a company that was doing innovative things in this space and really Human Longevity was the only place that I found that’s using imaging, genetics, peripheral blood biomarkers, plus family history and past medical history and putting it all together and getting a comprehensive view of health. So that’s what attracted me to the position. It’s been a wild ride and very interesting to see how the company has evolved and progressed and I think we have a pretty bright future. It’s exciting to be the medical director and that’s kind of how I ended up here.
Looking at this from a primary care perspective, if we could offer this testing at a very inexpensive price point to millions of people, how much better would our health improve overall? I think it could be pretty dramatic to be honest with you.
Longevity Blog (LB): I love that vision and one of the things that attracted me to HLI (Human Longevity Inc.) was one of your founders Peter Diamandis. He’s one of my… ‘heroes’, I’ll call him, a mentor, somebody I look up to. He shapes my thinking a lot and that idea of inexpensive testing for millions and reaching and impacting people positively is a mission that I believe in. The Longevity Blog is me playing my small part in helping to accomplish that.
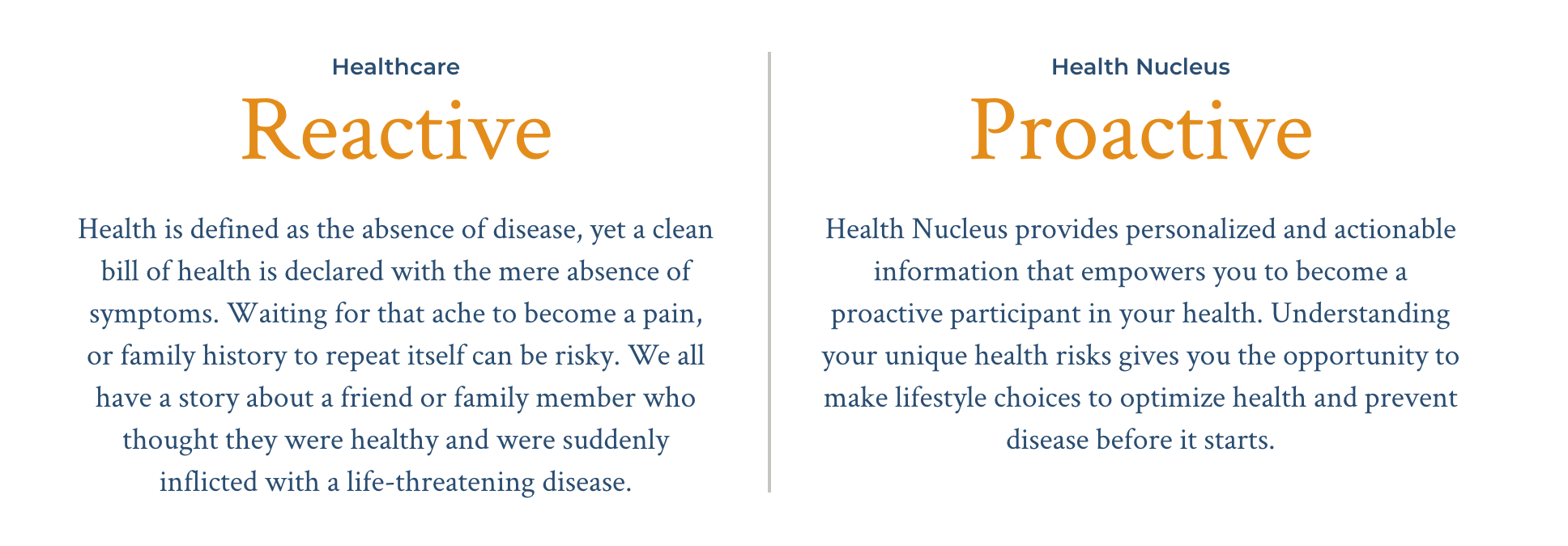
There’s a really interesting kind of dichotomy that we find between the healthcare industry and the Health Nucleus - and that’s thinking proactively about health care. If I were to go into my doctor’s office, my traditional GP here in Australia and didn’t have any acute symptoms of any sort and told them I was there to optimise my health, they would probably tell me to get outta there because they are there to take care of somebody who’s sick.
Q: So, I was curious what you think the Health Nucleus definition of “healthy” is and how might it be different from a traditional one?
From the Health Nucleus website
Dr Duchicela:
A: I think right now we are in version one of this, in that we are trying to create a suite of testing modalities. We are trying to detect the things that prematurely end people’s lives very early on. The broad categories of these would be things like cancer, metabolic diseases like aneurysm or heart disease, and neurodegenerative disease like alzheimer's. And right now our testing packages or testing suites are set up where we’re looking for those big categories of disease.
When we have enough data and we have enough people go through, and we are able to create advanced risk prediction tool kits and algorithms, that’s when the real promise of a company like this can come to fruition. We do get pretty rigorous metrics from things like genomics and also from the imaging biomarkers like liver fat and visceral fat, but what we really want to do and what we’re currently working on and what really excites me is taking your genomics - let’s say dementia or Alzheimer’s - taking your ApoE status and taking your hippocampal volume metrics from your imaging and also taking into account these other genomic variants that may not contribute to risk in such a large way as for example ApoE does, but on their own could tilt the needle one way or the other and putting this all together with your alcohol consumption, your BMI, your visceral fat levels and everything else and using machine learning and AI to come up with a ten year risk prediction for Alzheimer’s disease.
An example of the brain imagery data collected by MRI at the Health Nucleus, to compute metrics like hippocampal volume. Pictured: my own brain!
That’s where I think the true promise of this testing lies, but those algorithms need to be developed and it really does take a large data set to develop those algorithms. So right now I’d say in terms of our testing modalities we have a really good screening test for these five big categories of disease, but we really want to evolve into becoming the crystal ball for alzheimers, the crystal ball for metabolic disease, the crystal ball for prostate cancer or breast cancer by putting these algorithms or data modalities together and really deriving some good inferences from them, but we need a large data set first. I think that’s the biggest challenge with this.
LB: Right and so that kind of definition of healthy is actually shifting perspective out ahead of time almost, not just are you healthy now, but will you be healthy in the future and what can we do to minimise your risk and hopefully be able to be more predictive with more data and better algorithms that you’re continuing to develop.
Dr Duchicela:
it’s tricky to give a one size fits all definition of health. You really have to take in the context of the individual and see what their values and priorities are and what they want out of their life
A: Yeah and everyone really has their own definition of healthy, because different people have different values. For example I had a patient the other day who is a wine entrepreneur. This is his business, this is how he supports himself and his family, and to tell him, “Hey listen, if you really want to optimise your health and be quote-unquote completely healthy, you may want to avoid the amount of alcohol you’re drinking, because alcohol is a carcinogen.” For him, that would actually negatively impact his lifestyle. He wouldn’t necessarily be living a happy life if he gave up his profession. So, I think it’s tricky to give a one size fits all definition of health. You really have to take in the context of the individual and see what their values and priorities are and what they want out of their life.
And if you ask people about this, it’s not one size fits all. I think that’s the art of this, figuring out what drives them, what motivates them to come in to get assessed; Is it a family member who was recently diagnosed? Is it because they have a grandchild now and they want to be able to be healthy and active for when they get older?
And, at least as a physician that’s what I’m trying to focus on, how do we judge success? I don’t think it’s necessarily just not dying at an early age. It’s essentially living a fulfilling life and accomplishing the goals that you want to accomplish, whether that be having your own wine business and doing that as a profession or living to 100 and being cancer free the entire time. So, I think what we like to do here at the Health Nucleus is focus on the goals of the patient and really try to tailor our recommendations and counseling towards their goals.
LB: That’s great and I love that individual nature of it and the reflection of values and goals that the individual has. You’re right that the definition of healthy has to sit in that spectrum. That’s an encouraging answer and one I definitely agree with.
You just mentioned at the end of your talk there, cancer. Cancer is actually something that has personally impacted me, even directly in my own wife who has had to have two big peritonectomy surgeries for appendix cancer, thankfully she’s in remission now.
I think about the widespread availability of Health Nucleus technologies and MRI scanning etc. and think about if we had had routine access to something like that, how might that outcome have been different.
Q: Now, I don’t want you to go into theoretical outcomes for my specific case, but I’m really interested in helping to share with folks how the Health Nucleus can detect the actual presence of cancer, not just cancer risk but the actual presence of cancer at an early stage.
Dr Duchicela:
A: That’s a great question. When looking at our testing modalities, we have the imaging which is almost like a point-in-time disease test. We’re looking for disease right now, or early early disease, that’s the hope. With the genetic testing, it’s more your disease risk five years, ten years down the road. So the imaging is really powerful in that we can tell you within a few hours after a scan, if there is something concerning, a soft-tissue mass or an aneurysm even.
our goal is to develop a test that doesn’t use radiation, that we can give safely to many many people, that covers most cancers and then have a suite of tests to fill in the gaps essentially.
With our imaging, that’s really the goal, we cover some cancers pretty well, but we also have some gaps in our cancer coverage, just to be completely transparent. We don’t pick up colon cancer or certain other GI cancers very well, the MRI results are limited because we don’t have people do a bowel prep ahead of time, so we would still recommend a colonoscopy or a Cologuard test for that.
Certain pulmonary cancers you can’t get too well just yet with MRI but we’re working on that. No screening test is perfect, and you can’t catch every cancer with one single test, but our goal is to develop a test that doesn’t use radiation, that we can give safely to many many people, that covers most cancers and then have a suite of tests to fill in the gaps essentially.
My own Health Nucleus MRI scan (pictured), from 2018.
Or maybe they can go through their traditional medical provider to do the colon cancer screening if we don’t have a good option for it here. So in terms of developing a test for cancer, it’s tricky because we don’t want to say that if you have a completely clear scan you’re cancer free, there are gaps and limitations with the current technology. But over time as we are able to get more patients through, we’re able to do better processing on the images, so hopefully we will start to fill in those gaps with better early detection of cancer.
LB:
Q: You’ve made very clear caveats on the limitations there, but where does your technology excel and succeed? There would definitely be some anecdotal examples of detecting certain types of cancer at an early stage. You certainly have some excellent technology in that space, could you elaborate a bit further on that?
Dr Duchicela:
I think where it excels is that we’re able to get really good images without having to use contrast and that’s really important if we’re trying to scale this and bring it to many people at a low price point, we want to make it safe too. We do have pretty good post processing.
Let’s take prostate cancer for example, most men will die with prostate cancer, rather than from prostate cancer. So the trick is, how do we know which prostate cancer is going to be an issue and is going to prematurely end your life and which is so slow growing that they will most likely pass away from other things instead of the prostate cancer. With the post processing that the computer scientists and radiologists, people much smarter than myself, have developed, they’re able to light up and differentiate with the software these higher grade lesions in the prostate that have a higher chance of being a concern and being more aggressive and truly cancerous.
Image Credit: UC London. Prostate cancer screening by MRI is becoming more widely accepted. That’s very good news for early detection and treatment. Source
So that kind of differentiation on the back end is really powerful. We don’t want to be detecting things that won’t really harm someone in the long run. If you’re familiar with prostate cancer screening in general, it’s pretty controversial just because if we find something, we are almost obligated to biopsy it and there can be complications with biopsy. So we really want to make sure that we are finding things that are meaningful, and I think with the post processing that we do with our scans we can make that differentiation and better guide them to say alright this a lesion that is at a much higher risk, so we would suggest you get a biopsy, as opposed to alright this is lower risk lesion based on our scans and it may be more reasonable to watch and wait, get a serial PSA, that sort of thing.
LB: That makes a lot of sense, and you’re right in terms of wanting to minimise false detection or follow up treatment or biopsy to the really significant or possibly progressive forms of the cancer. That’s really fascinating.
We’ve talked a little bit about cancer, another big killer and one that is kind of a function of how old you are and how long you’ve been alive and a number of genetic risk factors is actually cardiovascular disease and in particular atherosclerosis.
I understand my risk as a man in his thirties is low for an acute event now, but that it’s really decade on decade buildup of plaque and inflammation and wear and tear on the arteries that increases the risk…
Q: So how does coming to the Health Nucleus help inform someone about their risk as they get older and what they can do as a young person to minimise the risk of atherosclerosis and cardiovascular disease?
I’ve split this interview into four parts, due to its length! Part 2 is coming soon :)
Note: the Health Nucleus has recently appointed a new Medical Director - Dr. Pamila Brar. Dr. Duchicela has transitioned to a role as full-time physician at the Health Nucleus, working directly with patients to optimise their healthcare!
Follow us on Twitter for the latest #Longevity news!
-
RT @nickengerer: Join a team, do a sport. Staying fit is easier with a clear purpose Bonus: you just might live longer Pic: Byro… https://t.co/L5yHxHJXas
-
Calcium AKG Alpha Keto Glutarate Supplement Review https://t.co/K7keDM3Lyn
-
Mitopure Review - Does this Urolithin A supplement actually work? https://t.co/0Y6Bx4yA7h
-
How Fast are You Aging? A Biological Age Test for Rate of Ageing with Ryan Smith of Trudiagnostic (Part 2) https://t.co/5SZW3Or6JJ
-
What is the Most Accurate Biological Age Test? An Interview with Ryan Smith of Trudiagnostic (Part 1) https://t.co/wdIxtTVeq0
-
One Skin Review - Self-Experiment Before and After Results with OS-01 https://t.co/3hqzLtfVa3